Birth Control Options in 2018
Written by Sara Langer
Photography by Illustration by Alessandra Olanow
Of the 61 million women of child-bearing age in the U.S., about 60% are currently using some form of birth control. There are about 20 different types of birth control, including hormonal or non-hormonal, one-time use, short-term, and long-term options. Since 1982, the pill and sterilization have been the most common option for birth control in the U.S., while there has been a steady increase in the use of other types of hormonal contraception as new options have entered the market. In addition, many women are searching for alternative methods and non-hormonal birth control.
Historically, insurance has been required to cover all FDA-approved contraceptives, but with the recent confirmation of Judge Kavanaugh to the Supreme Court and Trump’s changes to Title X and defunding Planned Parenthood earlier this year, the ability to access a diverse range of birth control options that are covered by insurance may be affected. In fact, most likely in reaction to the election of Trump and his campaign threats, there was a 19% rise in women scheduling appointments to discuss getting an IUD in November and December of 2016. And it is no wonder that women are feeling scared for what the future holds when it comes to making choices about our bodies. According to research by Guttmacher Institute, “The ability to delay, space, or avoid childbearing is crucial to women’s social and economic advancement.” So now, more than ever, it is important to understand what your birth control options are, how they work, and how much they might end up costing.
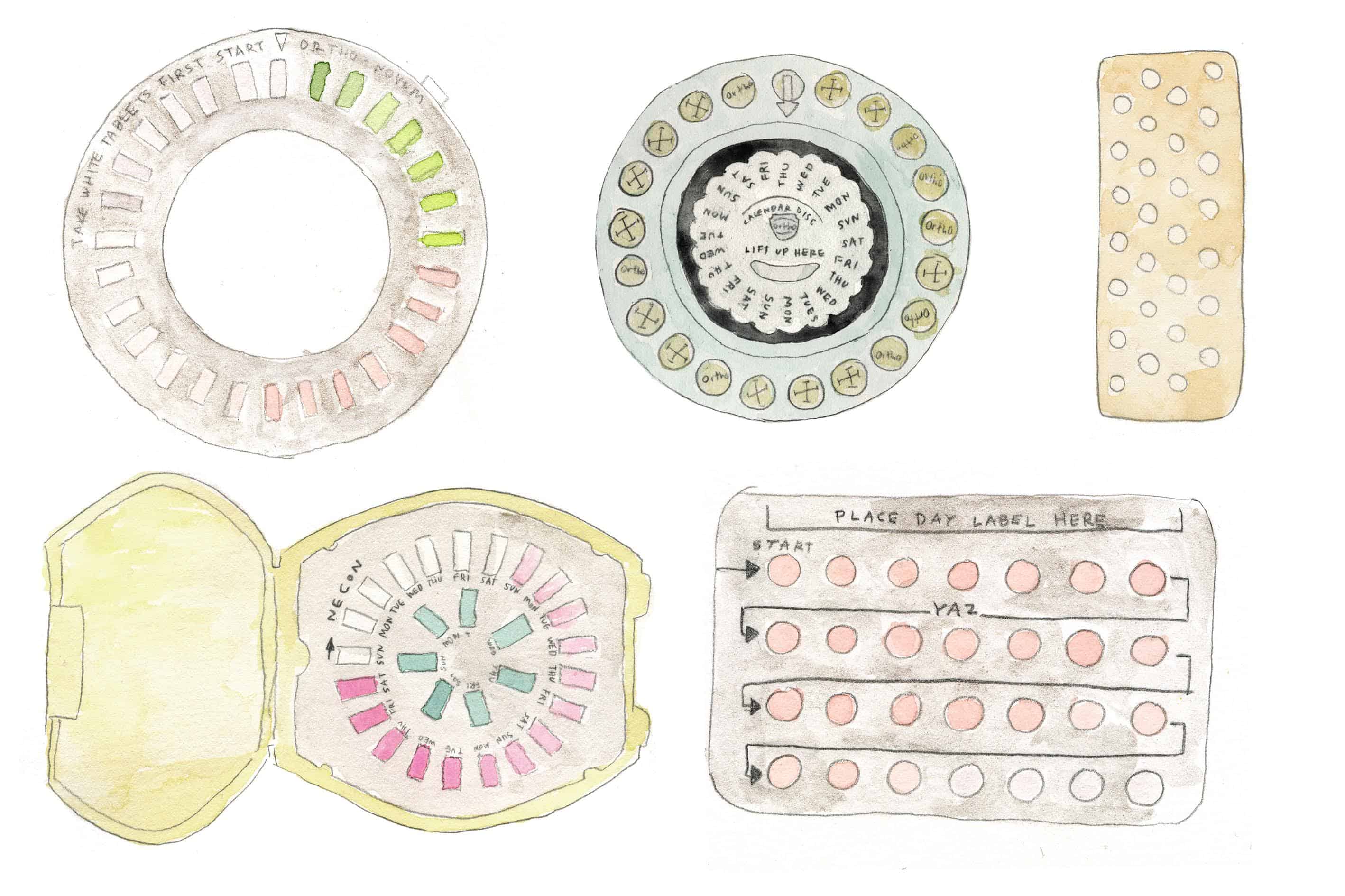
The Pill
Oral contraceptives, better known as birth control pills or simply “the pill”, are taken daily, releasing hormones that stop your ovaries from releasing eggs. Four out of five sexually active women have tried some type of birth control pill. The most common pill uses a combination of estrogen and progestin. A monthly combination pill pack contains 3 consecutive weeks of hormone-based pills and a week of placebos. The week you take the placebo pills is when you will get your period. The other option is a progesterone only pill, better known as “the mini-pill”. These pills do not have estrogen in them and are often prescribed to patients that may be sensitive to combination pills and the side effects. The mini-pill releases a small amount of progestin every day of the month and you do not get a period. When birth control pills are taken correctly they are over 99% effective in preventing pregnancy. The mini-pill is reportedly slightly less effective. Side effects vary, but they can range from unnoticeable to life-altering. While the pill is the most popular form of female contraception, other than permanent sterilization, the use of the pill has been on the decline as many women look for lower or no-hormone options or longer-term solutions. Since there are so many pill options out there, it’s best to weigh all of your options with your doctor. And while it might take your body a while to adjust to its normal ovulation cycle when you stop your birth control, it is possible to get pregnant within a month of stopping oral contraceptives or it may take months to return to your regular ovulation. It’s all specific to your individual body and cycle. Most all insurance plans still cover the cost of the pill, but if you are required to pay out of pocket, you can pay anywhere from $5 to $50 a month.
IUD
An IUD, or intrauterine device, is a small T-shaped device that is inserted into the uterus in order to prevent pregnancy. There are currently five IUDs on the market in the U.S., providing long-term birth-control, lasting anywhere from three to ten years. There are four hormonal IUDs available in the U.S.: Mirena, Skyla, Kyleena, and Liletta. These tiny plastic devices prevent pregnancy by releasing a small amount of the synthetic hormone progestin, which thickens cervical mucus, in order to block sperm from entering the uterus. It can also prevent eggs from leaving the ovaries. Paragard, the only non-hormonal option, is made of plastic and copper. Copper wire is coiled around the IUD and produces an inflammatory reaction that is toxic to sperm and eggs. Women who choose the hormonal IUD often report lighter or no period bleeding, while those with the copper IUD may experience heavier periods and more cramping. Paragard is not recommended for women with heavy periods or conditions like PCOS. Women with both types of IUDs have reported that the insertion process can be painful and cause temporary cramping and spotting, but the removal process is much less painful or even painless. IUDs do no prevent against STDs and without insurance they can cost over $1,000 out-of-pocket. While IUDs have been deemed safe for women as young as teens, they are most often prescribed to women who have already had at least one child. A study performed by Planned Parenthood found that female health providers were most likely to choose an IUD when it came to their own personal contraception choices.
Fertility Awareness
Fertility awareness methods are ways to track your ovulation in order to prevent pregnancy. These methods are often known as “natural family planning” or “the rhythm method”. One way women may do this is by tracking their daily body temperature. Normal body temperature is about 96 to 98 degrees Fahrenheit before ovulation. Immediately after ovulation, the body temperature can rise slightly, to 97 to 99 degrees Fahrenheit. It is recommended that you wait three days after a rise in temperature to have sex if you are wanting to prevent pregnancy. Checking and charting your cervical mucus is another way you can track your ovulation. Both temperature and cervical mucus tracking can take some time to figure out and you need to remember that your body can be easily affected by your environment and stress levels. Women who have predictable cycles may use the Calendar Method, or charting your menstrual cycle on the calendar. It’s best to do this for at least 6 months before you have unprotected sex if you are trying to avoid pregnancy. Fertility Awareness Methods are about 76% to 88% effective, according to Planned Parenthood. There are many apps out there, including the controversial, but highly rated Natural Cycles, which promotes itself as a form of non-hormonal, non-intrusive contraception. “Women input information about their menstrual cycles and body temperature into the app, and it uses algorithms to predict which days they are at risk of getting pregnant in the event of unprotected sex,” The Guardian recently explained. While some are arguing the efficacy of these statements and millennial’s blind trust in technology, “the popularity of Natural Cycles and women’s willingness to use it is not merely another ‘tech hype’ tale. It tells us something very important about the future of contraception and what women want: we are ready for something that disrupts neither our hormones, our moods, nor our pleasure.” Natural Cycles cost $79.99 for a one-year membership.
Male & Female Condoms and Diaphragms
Condoms, specifically male condoms, are the most easily accessible form of birth control and STD protection (other than abstinence) and are about 85% effective at preventing pregnancy. You can find condoms made out of latex, polyisoprene, nitrile, polyurethane, or lambskin. Non-latex options are considered to be less effective as they tear more easily. While the non-latex varieties are pretty basic, there are hundreds of varieties of the latex-options, varying in size, shape, texture, color, flavor, and with or without lubricants or spermicide. The much less used and available female condom is considered 95% effective when used correctly, but has a 21% failure rate as it can be difficult to get in place correctly. A nitrile (soft plastic), pre-lubricated pouch is inserted inside the vagina, much like you would insert a tampon, and it prevents sperm from reaching the egg. Female condoms are about twice as expensive as male condoms and not as readily available. Meanwhile, a diaphragm is a silicone dome or cup-shaped barrier, that is inserted into the vagina before sex in order to block sperm from entering the cervix, much like a female condom. You must keep the diaphragm in for at least 6 hours, to ensure sperm does not enter the cervix. It should be removed no more than 24 hours after insertion. Diaphragms come in different sizes, so you must be fitted by your doctor. Without insurance, they can cost up to $250 and it’s recommended they are replaced every year. Diaphragms have similar effectiveness as condoms, around 85%, but they do not protect against STDs and STIs. It is recommended that you use a diaphragm with spermicide (more info below) to make it even more effective.
The Implant, The Shot, The Ring, and The Patch
There are four other hormonal birth control options in addition to the pill and IUD, though less popular. The shot (Depo-Provera), the patch (Xulane), and the ring (Nuvaring or Annovera) all release estrogen and progestin into a woman’s body, while the implant (Nexplanon) only releases progestin. The shot and the implant are both LARCs, or long-acting reversible contraceptives, which provide effective contraception for an extended period without requiring user action, similar to an IUD. The shot is effective for three months, while the implant, which is implanted under the skin in the upper arm, is effective for up to three years. They can cost up to $100 and $800, respectively. The Nuvaring is a small and flexible circle that is inserted into the vagina and must be replaced monthly. Annovera is a new hormone-releasing vaginal ring that was approved by the FDA in August. Like Nuvaring, Annovera is placed in the vagina for three weeks followed by one week out of the vagina, at which time women may experience a period. The difference is with Annovera, the same ring can be put back into the vagina every month for one year, whereas Nuvaring must be replaced every month. The patch is highly effective, like the other hormonal contraceptives, but is the most short-term option as it must be replaced every week. These methods are about 90%-95% effective.
Spermicide, Cervical Cap, and The Sponge
Less popular and less effective, these three options are all hormone free, but don’t protect against STDs. On average they are around 75% effective when it comes to preventing pregnancy. The cervical cap does exactly what it sounds like it does—it creates a barrier so sperm cannot get into the cervix and is inserted into the vagina before sex. It is similar to a diaphragm but has a smaller shape and it can be left in the vagina for up to two days. It is recommended that you use Spermicide, a chemical that you put into your vagina right before sex. Spermicide works by blocking the entrance to the cervix and it slows downs and stops sperm from moving well enough to swim to your egg. The Sponge is small, round, and made from soft plastic. You put it deep inside your vagina before sex. The sponge covers your cervix and contains spermicide, so essentially is combines spermicide and the cervical cap into one product. The Sponge and spermicide are both available over the counter.
Sterilization
This is the only form of permanent, irreversible birth control for women, and also one of the most common types of birth control in the world. Sterilization, or tubal ligation, is a surgical procedure that permanently closes the fallopian tubes, and is often referred to as “getting your tubes tied.” Tubal ligation is a routine medical procedure, but male sterilization, or vasectomy, is a less invasive procedure with fewer risks and complications. Tubal ligation can be performed with local or general anesthesia, although local is considered safer and can be done at any time, including after childbirth or in combination with another abdominal surgery, such as a C-section. Sterilization has a dark side in history around the world, including dangerous mass sterilization practices. Without insurance, sterilization can cost up to $6,000.
Share this story



