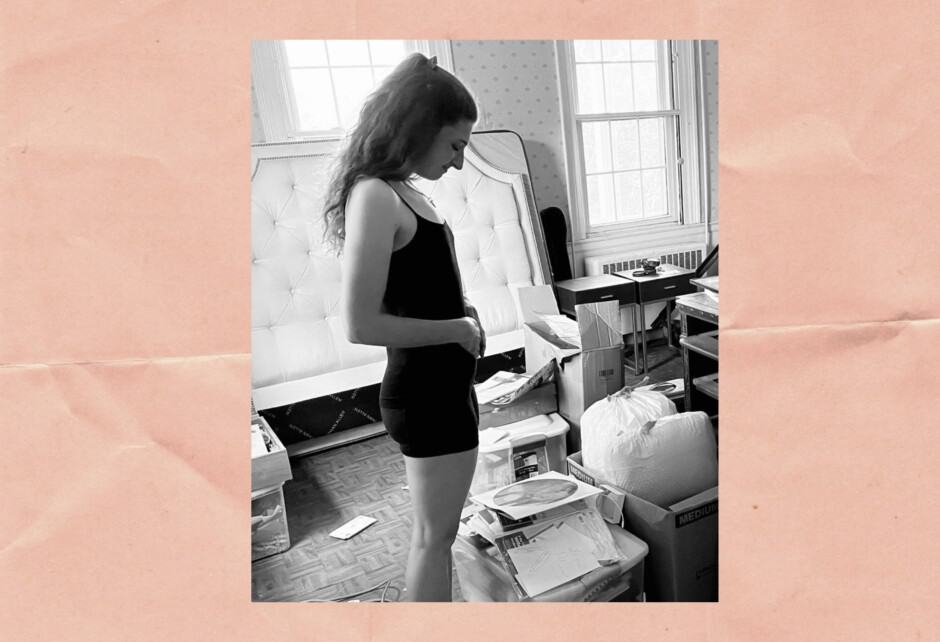
Why I Quit My Career After Surviving A High Risk Pregnancy
Written by Parijat Deshpande
Photography by Photo by Samantha Estrada
October marks Pregnancy & Infant Loss Awareness Month and today we’re bringing you the story of a woman who’s made it her mission to help moms-to-be brave a pregnancy after loss. Parijat Deshpande is the CEO of a boutique company dedicated to reducing pregnancy complications and ending preterm birth. A pregnancy loss survivor herself, she’s also the author of Pregnancy Brain: A Mind-Body Approach to Stress Management During a High-Risk Pregnancy. Below she shares a bit about her story of surviving a high risk pregnancy and why she’s devoted to helping others do the same.
After her own experience with high-risk pregnancy, Parijat went from patient to practitioner to help other women beat the statistics—a journey she chronicled in her bestselling book, Pregnancy Brain: A Mind-Body Approach to Stress Management During a High-Risk Pregnancy. Today, she continues to take a trauma-informed, neurobiological approach to reproductive health to help her concierge-level private clients improve pregnancy outcomes after preterm birth or late-term loss. Parijat also consults with medical clinics, NICUs, antepartum and labor and delivery units, training them to optimize patient satisfaction and improve patient outcomes by leveraging trauma-informed patient and family-centered care
I remember it like it was yesterday. I was stuck at home during the summertime when the weather was beautiful and everyone else I knew was at work or in grad school and busy with their lives. I was alone at home, stuck indoors, on modified activity restrictions because of my high-risk pregnancy.
I didn’t realize then just how much more high-risk my pregnancy would become.
I wasn’t used to being alone without anything to do. I loved being busy with a calendar full of professional, personal, and social happenings. Now, suddenly, I had everything wiped off of my to-do list and calendar and was forced to be at home and do less. It was all so foreign to me not only because I was used to being busy, but because the distractions of Netflix binges and fiction novels weren’t helping with the very real fear I was living with of losing another child.
My first pregnancy ended abruptly when I was rushed to the emergency room due to a ruptured ectopic pregnancy. I didn’t know at the time that ruptured ectopic pregnancies are actually one of the most dangerous experiences for women who are trying to conceive and trying to be pregnant. Now, in my second pregnancy after getting pregnant from IVF, I was not only having to reconcile that I had just survived a life-threatening experience, but also live in the reality that I could potentially lose a second child.
One afternoon, as I sat at home, the light flooding through the floor-to-ceiling windows behind the sofa I was parked on for weeks, I remember thinking I need support. I need help. I was feeling helpless, like I would do anything in the world to help this baby but had no idea what that could be. I felt like my hands were tied and I was angry. I had done everything right: I had taken all the prenatal vitamins, attended all my appointments, ate healthily and exercised (before I was asked to stay home and stay off my feet) regularly. Why was this happening to me, to us?
I knew I needed help and support but I didn’t know where to turn. As someone who was trained professionally in clinical psychology, I knew what response I would get if I contacted someone like me—a counselor or therapist. I knew what they would say to try to calm my anxiety; they’d try to help me shift my thoughts from fear to positivity, teaching me to cope with my anxiety or validate my feelings without giving me something actionable to do to actually help me stay pregnant. Now that the roles had switched and I was the patient—the mother feeling this fear and the mama-bear instinct to protect this child—I knew that calming down or changing my thoughts wasn’t at all what I wanted or needed.
I didn’t want coping strategies for my anxiety or advice on how to breathe deeply. What I wanted and needed was to learn how to protect my pregnancy from my fear of losing another child. I wanted to know that it was normal and even expected that a person who is pregnant after a loss is going to be scared—and that it was a waste of my energy to try to focus on minimizing the fear.
I wanted to know: How do I protect my pregnancy, my life, and my baby?
I didn’t know of a single person who was doing that work. I definitely didn’t know anyone who was doing this from a body-based perspective—from the angle or perspective of normalizing the somatic experience while also showing that there is a way to improve your odds of staying pregnant. It was that experience, along with so many more in the months after, like landing in the hospital during the periviable stage and being told to prepare ourselves to lose our child, that led me to the work I do today.
The Wednesday before our son was born at 24 weeks and 5 days, I made a vow to him and myself that if we both survived, I would change my career. I vowed that I would leave everything behind from my then role as a child and family therapist and undergraduate Psychology Lecturer at UC Berkeley to become that person I needed during my pregnancy. I would be someone who understood and normalized the experience and the fears of being pregnant after loss and also had the science, biology, and research to back up how pregnant people can influence their bodies to help themselves stay pregnant, reduce the risk of complications, and reduce the risk of preterm birth.
I have done just that. I left everything behind to become the person I needed back then and that so many others navigating pregnancy loss, preterm birth, and high-risk pregnancy need now. In the past few years, I’ve been able to walk alongside and support hundreds of pregnant people to help them stay pregnant, beat medical odds, and reclaim a trust in their bodies that they thought was eroded forever. If there’s one thing I hope you take away as you are going through your pregnancy loss, preterm birth, or high-risk pregnancy, it’s this: this was not your fault. You did nothing wrong to deserve this. And also, there is SO much hope for the future for a different experience next time—hope that’s based in science and neurobiology.
Are you a mother with something to say? Send us an email to be considered for our “Mom Talk” column.
Share this story